MODERNA - L' étude toxicologique du vaccin ne respecterait pas les bonnes pratiques de laboratoire
De : https://threadreaderapp.com/thread/1446617987390349312.html
Via : ZAZA40
UN AVIS DE SPÉCIALISTE
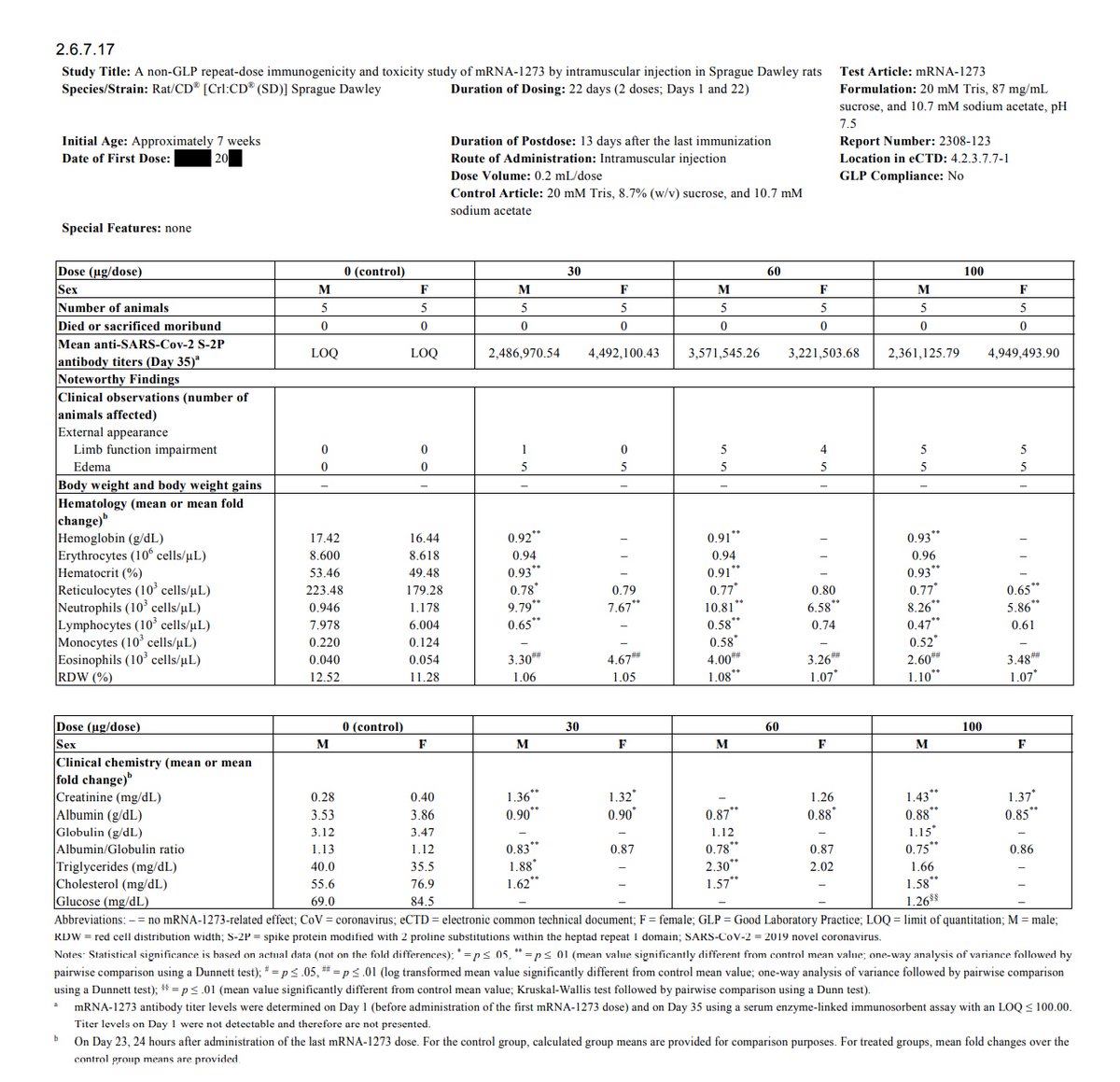
1/8 Faut-il en rire ou en pleurer. Dans son rapport soumis à l'EMA pour obtenir son AMM conditionnelle fin 2020, l'étude toxicologique de Moderna pour son mRNA-1273 (2308-123 ) ... est encore plus foireuse que celle de Pfizer pour son BNT162b2...
ema.europa.eu/en/documents/a…
ema.europa.eu/en/documents/a…
2/8 Moderna a décidé que son étude toxicologique 2308-123 ne respectait pas les bonnes pratiques de laboratoire ... c'est pas faux quand on voit comment ils se sont foulés ... une NFS et une biochimie sanguine ... 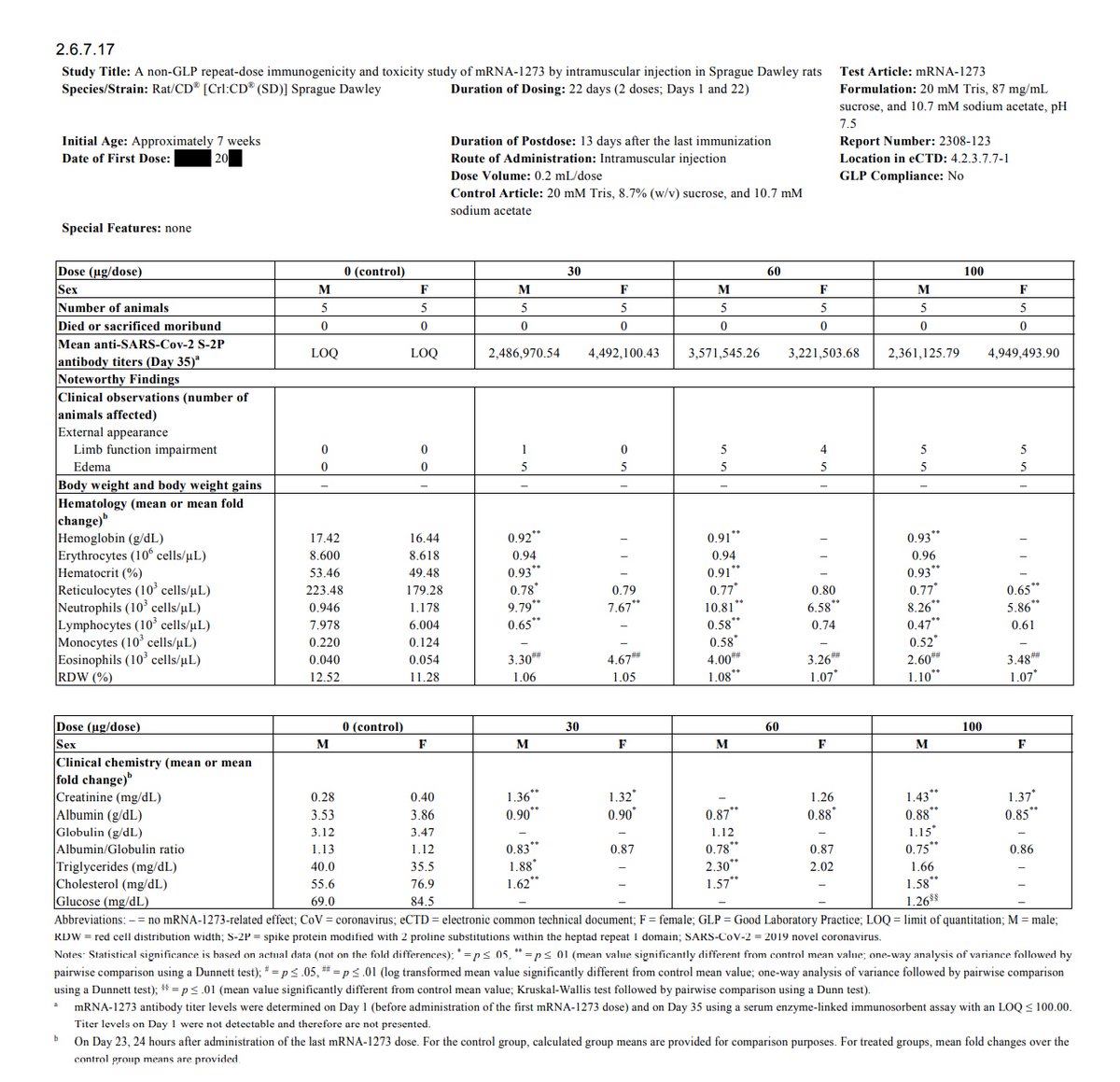
3/8 donc Moderna va déduire la toxicité de son vaccin en utilisant les vésicules lipidiques contenant des brins d'ARNm d'autres virus qui n'ont rien avoir avec la spike du SARS-Cov-2 (Zika, CMV, Influenza). 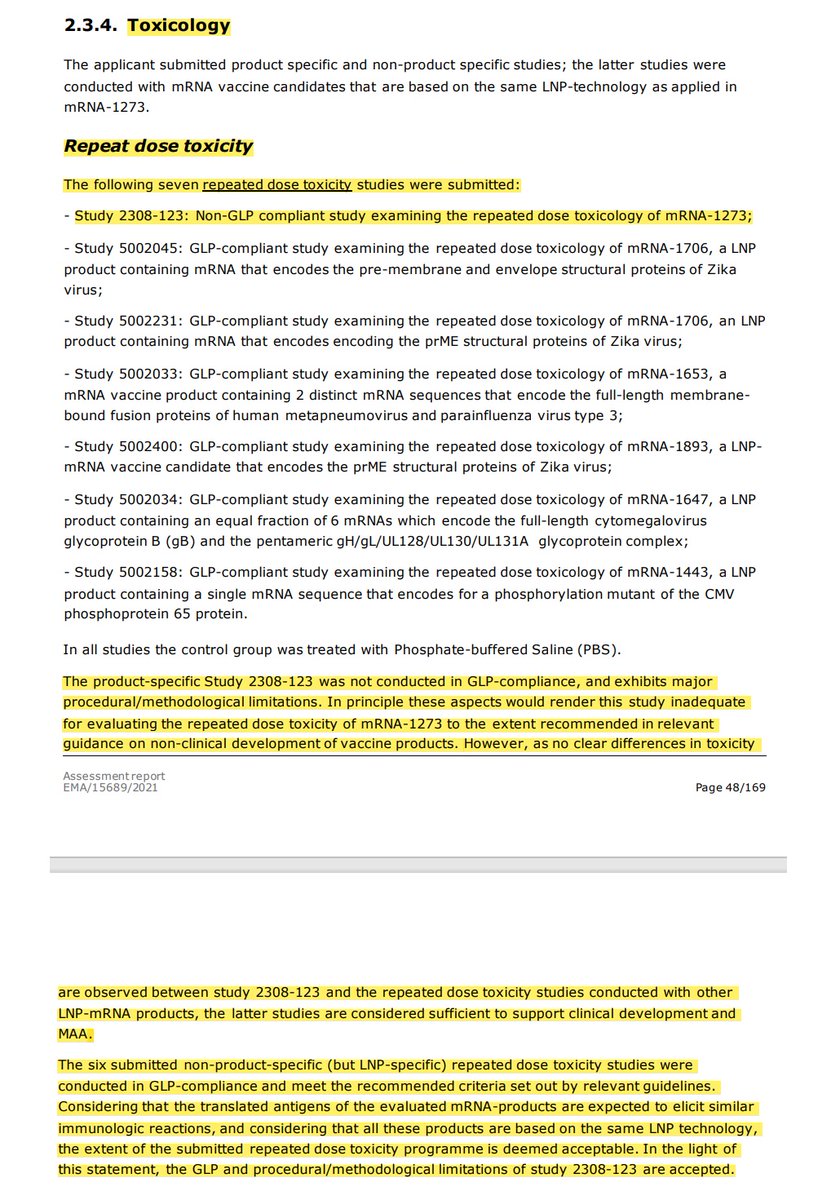
4/8 C'est connu! On peut connaître la toxicité de la digitale en administrant Matricaria chamomilla ... C'est logique! Sur cette base, de nombreux politiciens et médecins affirment que les vaccins à ARNm codant la spike sont sûrs et sans effets secondaires ...
5/8 Ils devraient alors être d'accord qu'on leur injecte 2x à 21j d'intervalle une dose de 150μg/kg d'ARNm pour finaliser l'étude toxicologique de Moderna? Les rats se portaient bien il paraît! Le recrutement est ouvert!
6/8 On sait que la spike vaccinale (S1 ou S totale) circule dans le sang jusqu'à un mois, que les vésicules lipidiques avec ARNm circulent dans le sang, que les vaisseaux sanguins de différents tissus peuvent exprimer la spike vaccinale avec réaction inflammatoire et lymphocytaire
7/8 Que la spike du SARS-Cov-2 est capable à elle seule d'induire une toxicité sur les cellules endothéliales, les macrophage, PBMCs, ... Alors, il est grand temps que ces politiciens, HAS, ARS et médecins de plateau qui n'y connaissent rien arrêtent de copiner avec Pfizer/Moderna
8/8 et que l'on propose des méthodes de vaccination plus sûrs où l'on administre une dose contrôlée... par exemple un vaccin inactivé ou un vaccin vivant atténué intra-nasal comme nous utilisons pour les coronavirus en médecine vétérinaire.
Vaccination against coronaviruses in domestic animals The current pandemic of COVID-19 has set off an urgent search for an effective vaccine. This search may well benefit from the experiences of the animal health profession in the development and use of … https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC7284272/
ahajournals.org/doi/10.1161/CI…
Lei et al. SARS-CoV-2 Spike Protein Impairs Endothelial Function via Downregulation of ACE 2. Circulation Research, March 2021.
Lei et al. SARS-CoV-2 Spike Protein Impairs Endothelial Function via Downregulation of ACE 2. Circulation Research, March 2021.
sciencedirect.com/science/articl…
Nuovo et al. Endothelial cell damage is the central part of COVID-19 and a mouse model induced by injection of the S1 subunit of the spike protein. Ann Diagn Pathol. April 2021.
Nuovo et al. Endothelial cell damage is the central part of COVID-19 and a mouse model induced by injection of the S1 subunit of the spike protein. Ann Diagn Pathol. April 2021.
Endothelial cell damage is the central part of COVID-19 and a mouse model induced by injection of the S1 subunit of the spike protein Neurologic complications of symptomatic COVID-19 are common. Brain tissues from 13 autopsies of people who died of COVID-19 were examined. Cultured en…https://www.sciencedirect.com/science/article/abs/pii/S1092913420302288?via%3Dihub
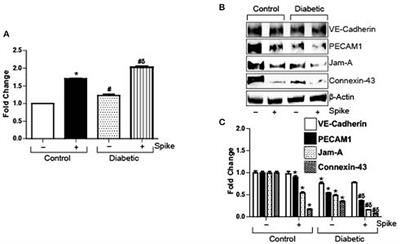
frontiersin.org/articles/10.33…
Raghavan et al., SARS-CoV-2 Spike Protein Induces Degradation of Junctional Proteins That Maintain Endothelial Barrier Integrity. Front Cardiovasc Med. June 2021.
Raghavan et al., SARS-CoV-2 Spike Protein Induces Degradation of Junctional Proteins That Maintain Endothelial Barrier Integrity. Front Cardiovasc Med. June 2021.
SARS-CoV-2 Spike Protein Induces Degradation of Junctional Proteins That Maintain Endothelial Barrier Integrity Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) uses the Angiotensin converting enzyme 2 (ACE2) receptor present on the cell surface to enter cells. Angiotensin converting enzyme 2 is pre…https://www.frontiersin.org/articles/10.3389/fcvm.2021.687783/full
biorxiv.org/content/10.110…
Avolio et al. The SARS-CoV-2 Spike protein disrupts human cardiac pericytes function through CD147-receptor-mediated signalling: a potential non-infective mechanism of COVID-19 microvascular disease. BioRxiv. July 2021.
Avolio et al. The SARS-CoV-2 Spike protein disrupts human cardiac pericytes function through CD147-receptor-mediated signalling: a potential non-infective mechanism of COVID-19 microvascular disease. BioRxiv. July 2021.
The SARS-CoV-2 Spike protein disrupts human cardiac pericytes function through CD147-receptor-mediated signalling: a potential non-infective mechanism of COVID-19 microvascular disease Severe coronavirus disease 2019 (COVID-19) manifests as a life-threatening microvascular syndrome. The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) uses the Spike (S) protein to engage…https://www.biorxiv.org/content/10.1101/2020.12.21.423721v2
pubmed.ncbi.nlm.nih.gov/34160250/
Meyer et al. SARS-CoV-2 Spike Protein Induces Paracrine Senescence and Leukocyte Adhesion in Endothelial Cells. Journal of Virology, August 2021.
Meyer et al. SARS-CoV-2 Spike Protein Induces Paracrine Senescence and Leukocyte Adhesion in Endothelial Cells. Journal of Virology, August 2021.
SARS-CoV-2 Spike Protein Induces Paracrine Senescence and Leukocyte Adhesion in Endothelial Cells - PubMed Increased mortality in COVID-19 cases is often associated with microvascular complications. We have recently shown that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spike protein promo…https://pubmed.ncbi.nlm.nih.gov/34160250/
pubmed.ncbi.nlm.nih.gov/34156871/
Colunga Biancatelli et al. The SARS-CoV-2 spike protein subunit S1 induces COVID-19-like acute lung injury in Κ18-hACE2 transgenic mice and barrier dysfunction in human endothelial cells. Am J Physiol Lung Cell Mol Physiol. August 2021.
Colunga Biancatelli et al. The SARS-CoV-2 spike protein subunit S1 induces COVID-19-like acute lung injury in Κ18-hACE2 transgenic mice and barrier dysfunction in human endothelial cells. Am J Physiol Lung Cell Mol Physiol. August 2021.
The SARS-CoV-2 spike protein subunit S1 induces COVID-19-like acute lung injury in Κ18-hACE2 transgenic mice and barrier dysfunction in human endothelial cells - PubMed Acute lung injury (ALI) leading to acute respiratory distress syndrome is the major cause of COVID-19 lethality. Cell entry of SARS-CoV-2 occurs via the interaction between its surface spike protein (… https://pubmed.ncbi.nlm.nih.gov/34156871/
ncbi.nlm.nih.gov/labs/pmc/artic…
Li et al. SARS-CoV-2 spike promotes inflammation and apoptosis through autophagy by ROS-suppressed PI3K/AKT/mTOR signaling. Biochim Biophys Acta Mol Basis Dis. August 2021.
Li et al. SARS-CoV-2 spike promotes inflammation and apoptosis through autophagy by ROS-suppressed PI3K/AKT/mTOR signaling. Biochim Biophys Acta Mol Basis Dis. August 2021.
SARS-CoV-2 spike promotes inflammation and apoptosis through autophagy by ROS-suppressed PI3K/AKT/mTOR signaling Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection-induced inflammatory responses are largely responsible for the death of novel coronavirus disease 2019 (COVID-19) patients. Howev… https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC8390448/
pubmed.ncbi.nlm.nih.gov/34445747/
Jana et al. Cell-Free Hemoglobin Does Not Attenuate the Effects of SARS-CoV-2 Spike Protein S1 Subunit in Pulmonary Endothelial Cells. Int J Mol Sci. A
Jana et al. Cell-Free Hemoglobin Does Not Attenuate the Effects of SARS-CoV-2 Spike Protein S1 Subunit in Pulmonary Endothelial Cells. Int J Mol Sci. A
Cell-Free Hemoglobin Does Not Attenuate the Effects of SARS-CoV-2 Spike Protein S1 Subunit in Pulmonary Endothelial Cells - PubMed SARS-CoV-2 primarily infects epithelial airway cells that express the host entry receptor angiotensin-converting enzyme 2 (ACE2), which binds to the S1 spike protein on the surface of the virus. To de…https://pubmed.ncbi.nlm.nih.gov/34445747/
pubmed.ncbi.nlm.nih.gov/34616396/
Barhoumi et al. SARS-CoV-2 Coronavirus Spike Protein-Induced Apoptosis, Inflammatory, and Oxidative Stress Responses in THP-1-Like-Macrophages: Potential Role of Angiotensin-Converting Enzyme Inhibitor (Perindopril). Front Immunol. September 2021.
Barhoumi et al. SARS-CoV-2 Coronavirus Spike Protein-Induced Apoptosis, Inflammatory, and Oxidative Stress Responses in THP-1-Like-Macrophages: Potential Role of Angiotensin-Converting Enzyme Inhibitor (Perindopril). Front Immunol. September 2021.
SARS-CoV-2 Coronavirus Spike Protein-Induced Apoptosis, Inflammatory, and Oxidative Stress Responses in THP-1-Like-Macrophages: Potential Role of Angiotensin-Converting Enzyme Inhibitor (Perindopril) - PubMedSuggested pathways that might be involved at least in part in S protein inducing activation of inflammatory markers (red narrow) and angiotensin-converting enzyme inhibitor (ACEi) modulation of this p…https://pubmed.ncbi.nlm.nih.gov/34616396/
pubmed.ncbi.nlm.nih.gov/34572407/
Rotoli et al. Endothelial Cell Activation by SARS-CoV-2 Spike S1 Protein: A Crosstalk between Endothelium and Innate Immune Cells. Biomedicines. September 2021.
Rotoli et al. Endothelial Cell Activation by SARS-CoV-2 Spike S1 Protein: A Crosstalk between Endothelium and Innate Immune Cells. Biomedicines. September 2021.
Endothelial Cell Activation by SARS-CoV-2 Spike S1 Protein: A Crosstalk between Endothelium and Innate Immune Cells - PubMed Our data suggest that pro-inflammatory mediators released by spike-activated macrophages amplify the activation of endothelial cells, likely contributing to the impairment of vascular integrity and to…https://pubmed.ncbi.nlm.nih.gov/34572407/
pubmed.ncbi.nlm.nih.gov/34003736/
Han et al. ZMPSTE24 Regulates SARS-CoV-2 Spike Protein-enhanced Expression of Endothelial PAI-1.Am J Respir Cell Mol Biol. September 2021.
Han et al. ZMPSTE24 Regulates SARS-CoV-2 Spike Protein-enhanced Expression of Endothelial PAI-1.Am J Respir Cell Mol Biol. September 2021.
ZMPSTE24 Regulates SARS-CoV-2 Spike Protein-enhanced Expression of Endothelial PAI-1 - PubMedEndothelial dysfunction is implicated in the thrombotic events reported in patients with coronavirus disease (COVID-19), but the underlying molecular mechanisms are unknown. Circulating levels of the …https://pubmed.ncbi.nlm.nih.gov/34003736/
• • •





Commentaires
Enregistrer un commentaire